How the Bugs We Live with Could Help Fight Lung Cancer
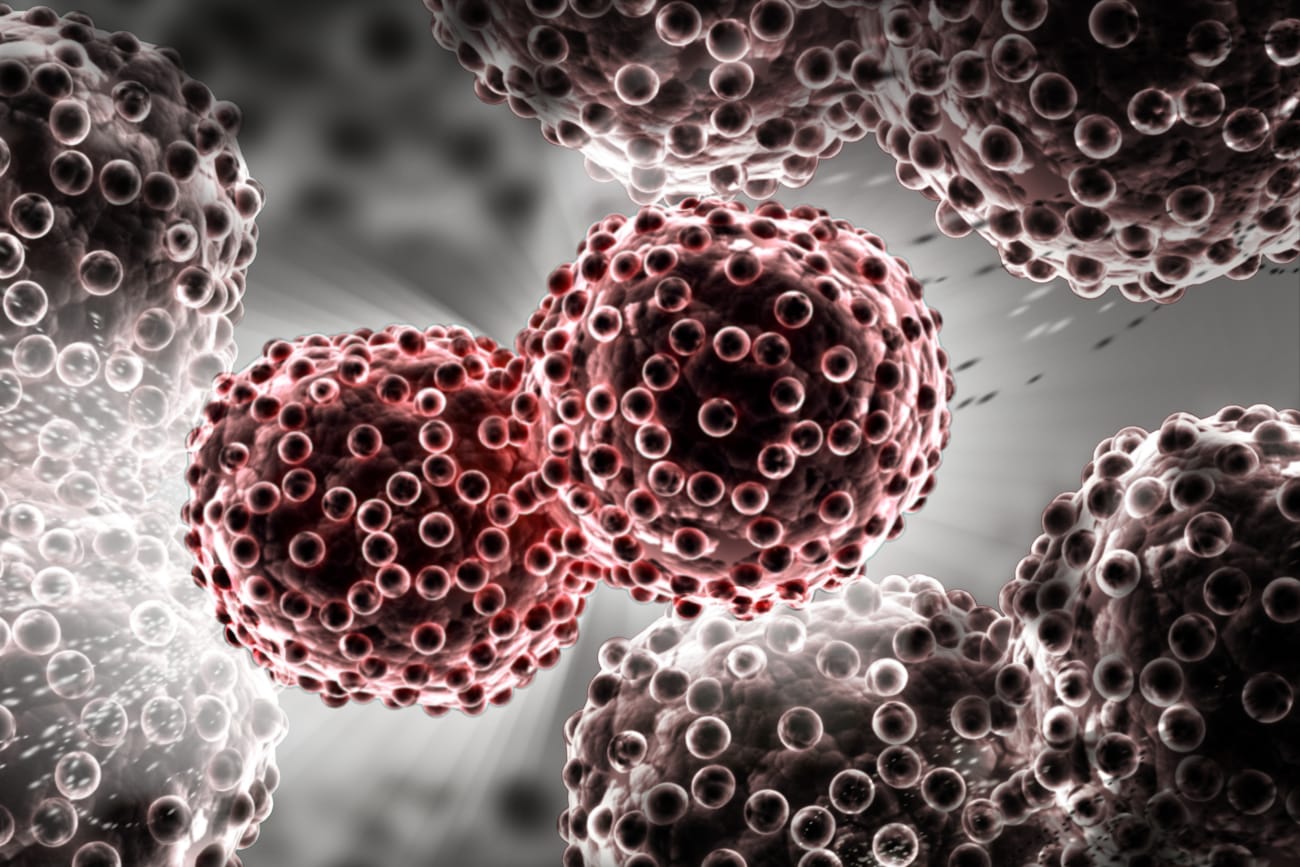
A new class of cancer-fighting drugs called checkpoint inhibitors is offering hope to patients with several kinds of solid tumors, particularly lung cancer and melanoma. The medications, which work by spurring the body’s immune system to attack tumor cells, prolong life in roughly 20 percent of people who take them.
Why some patients do well but others fail to improve is a mystery, but emerging evidence suggests that at least some of the reason may lie with the trillion-odd bacteria that make up the body’s microbiome.
Researchers at the Johns Hopkins Kimmel Cancer Center and Bloomberg~Kimmel Institute for Cancer Immunotherapy are studying how the microbiome—the menagerie of germs that live in the gastrointestinal tract and other organ systems, including the lungs and skin—may interact with checkpoint inhibitors in ways that both make the drugs stronger and that potentially weaken their effectiveness. Their goal is to identify which strains of bacteria sit on which side of the ledger, and, if possible, to tweak a patient’s microbiome in ways that make the cancer drugs even more potent.
Infectious disease and microbiome expert Cynthia Sears, M.D., is leading the research effort. “We’re trying to attack on multiple fronts,” says Sears.
Research in the area has heated up recently, with several publications showing that groups of bacteria may alter the function of immune cells in ways that intersect with the function of checkpoint inhibitors. Some experiments found that a greater abundance in the gut of certain species of bacteria was associated with a stronger response to the drugs. Others showed the opposite—species of microbes that, when present, were linked to a poor response to the immunotherapy drugs.
At the moment, the research is in early days, Sears says, with many questions remaining unanswered. Which species of microbes are most important in the interaction, and how they alter the way the body processes the cancer drugs, is unclear.
“One possibility is that there is priming, or education, of the immune system that either enhances or inhibits the capacity of the cells to respond to the tumor,” Sears says. In other words, the presence of certain bacteria in the intestines conditions the immune system the way regular exercise strengthens muscles. When checkpoint inhibitors unlock the power of the immune system, it’s better prepared to fight off cancer. Alternatively, exposure to certain strains of bacteria may sap the immune system, crippling T cells so that they’re unable to rally that defense.
Another possibility is that proteins that the bacteria in the gut make are similar to those produced by cancer cells. “In this idea, the patient’s immune system first develops an immune response to one or more bacterial proteins,” Sears says. “When the tumor is treated with checkpoint blockade, the immune system is released to attack the tumor using the antibodies against bacterial proteins that ‘mimic’ tumor proteins.”
Lung cancer expert Jarushka Naidoo, M.D., is collaborating with Sears on the project. She is helping collect samples of bacteria from patients being treated with immunotherapy, taking swabs from stool, fluid from the lungs—which have their own microbiome—the mouth, and urine. Using DNA profiling, they’ll catalog all of the organisms present and try to build a profile of which ones are linked to a good response to the drugs and which appear to hinder their effectiveness.
Although the research is still in its early stages, Sears says she hopes the work will lead to the development of therapies—such as a “microbe cocktail” or even a vaccine—that will boost the immune response in cancer patients who receive immunotherapy. “We want these drugs to work for most patients, not just a small percentage of them,” she says.
To discuss or refer a patient, call 410-955-LUNG.