
April 10, 2019
At Johns Hopkins, the management of patients with advanced heart failure is a team sport, with cardiologists and cardiac surgeons working in tandem with other providers to keep patients at the top of their game.
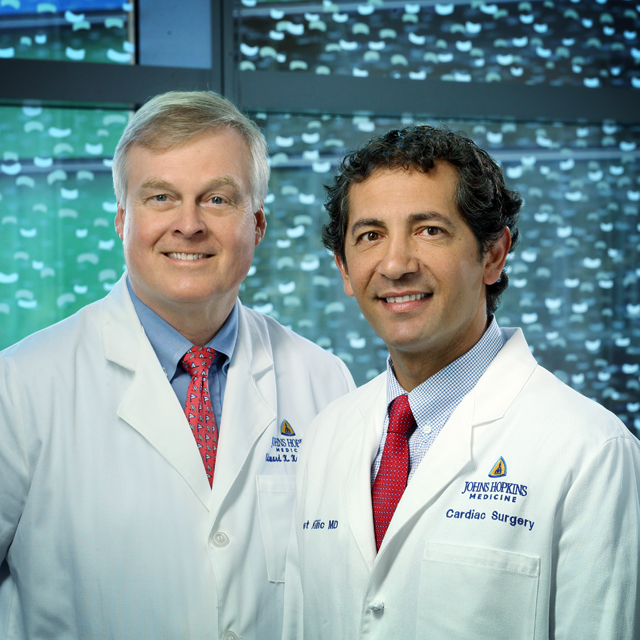
"Advanced heart failure (AHF) runs a spectrum of diseases, from your most common, lack of blood flow, causing heart failure to other nonischemic causes, such as valve problems, hypertrophic cardiomyopathy or amyloidosis,” says cardiothoracic surgeon Ahmet Kilic, director of heart transplantation and mechanical and circulatory support. “The uniqueness of Hopkins is that we have a specialist in every one of those major disease processes that lead to heart failure.”
“It’s a very close-working team and unit,” says AHF cardiologist Kavita Sharma, one of six such specialists (along with Edward Kasper, Ilan Wittstein, Steven Hsu, Nisha Gilotra and Roberta Florido) who meet daily with Kilic and care team members. These include transplant nurses, left ventricular assist device (LVAD) nurses, social workers, pharmacists, psychologists, and nutritionists. Together, they discuss current and incoming patients and their therapy plans, as well as confer on whether to accept donor hearts.
“It’s almost like having not just a second opinion, but third and fourth opinions on any given disease,” says Kilic. “That allows us to make real-time decisions in the benefit of patients.”
Share Fast Facts
Coordinated Care Improves Odds for Patients with Advanced Heart Failure Click to Tweet
Coordinated care starts from the moment patients are referred, says Sharma, with cardiologists driving the initial medical management and the multi-disciplinary team assessing patient candidacy for advanced therapies, including mechanical assist devices or transplants. The shared approach to care continues after surgery until patients are discharged, and even for follow-up care.
The cardiology team has varied clinical expertise, says Kasper, interim director of heart failure and heart transplantation:
- Ilan Wittstein, M.D.: Advanced Heart Failure Fellowship Program Director, with specialized interest in stress cardiomyopathy.
- Kavita Sharma, M.D.: Director of JHU Heart Failure with Preserved Ejection Fraction Program. The JHU HFpEF program has become one of the largest in the country.
- Nisha Gilotra, M.D.: Director of the Heart Failure Bridge Clinic, with special interest in inflammatory cardiomyopathies including cardiac sarcoidosis.
- Steven Hsu, M.D.: Research interest in right ventricular function and pulmonary hypertension.
- Roberta Florido, M.D., M.H.S.: Specialization in Cardio-oncology, the management of heart failure in patients treated for cancer.
The JHH Heart Failure Bridge Clinic is a nurse-practitioner led HF transition clinic, which bridges the gap between inpatient and outpatient management of HF patients, a vulnerable time in patient care. Kasper says: “Our nurse practitioners see patients within one week of hospital discharge, to ensure clinical stability, titrate medications as needed, and avoid readmission. It’s been a real boon to patients and the health care system.”
Ten to 20 years ago, AHF was as deadly as any cancer, Kasper adds. “These days, with the proper medications and advancements in technology with LVADs and transplants, it doesn’t necessarily have to be that way. Patients are doing better, feeling better and living longer.”

