The consequences of COVID-19 on fetal development are still unknown, and even less is understood about what those effects will be in combination with those of seasonal flu. That’s why Irina Burd, director of the Integrated Research Center for Fetal Medicine at Johns Hopkins Medicine, recommends that physicians caring for pregnant women consult a maternal-fetal specialist when confronted with concerns related to these viruses.
“I focus on HIV, Zika, cytomegalovirus and COVID-19 in pregnancy, and we don’t know what COVID-19 plus flu is going to mean yet,” says Burd, who is a professor in Johns Hopkins’ Department of Gynecology and Obstetrics, as well as neurology. Because of this, she welcomes providers to partner with her and colleagues at Johns Hopkins if they feel uneasy about the way a patient’s symptoms are presenting. “There need not be any heroic, individual moves. If a physician does not feel comfortable, all they need to do is pick up the phone. We will do all that we can to treat the patient and, as soon as the patient is clear, transfer her back to their care.”
Burd now leads a study in which she anticipates following more than 250 children born at Johns Hopkins to mothers who were COVID-19 positive. “It’s hard to say at the neonatal period that everything is fine with the fetus, but based on the children in the study group we found that COVID-19 did not touch them,” says Burd. However, she says, even if they don’t become infected with the virus that causes the disease, “inflammation in the mother may lead to neonatal effects and a spectrum of adverse neurobehavioral outcomes. Potentially, the effects of COVID-19 are going to be long term, and the echoes are going to be seen and heard for a long time.”
Research Focuses on Inflammation and Infection
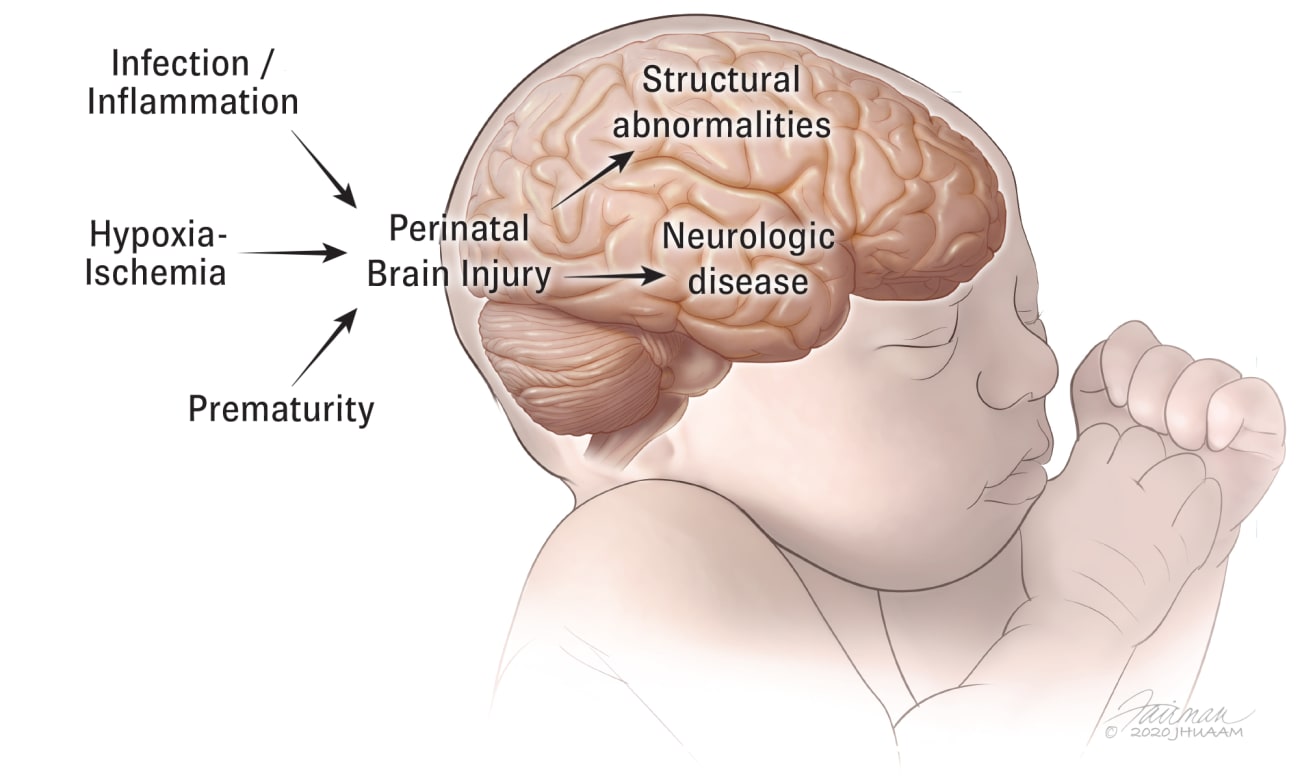
Recruited in 2011 to spearhead the development of fetal medicine and fetal neurology programs at Johns Hopkins, Burd is uniquely positioned to study how placental inflammation and infection affect fetal neuroimmune and immune development. Her research examines the pathogenesis of perinatal brain programming with exposure to intrauterine insults.
Funded by a National Institute of Child Health and Human Development (NICHD) grant, one study[i] established that exposure to intrauterine inflammation leads to placental inflammation, alters gray matter development, and culminates in long-term neurobehavioral sequelae in the surviving offspring. These studies were a springboard for further clinical, translational and basic science research.
Share Fast Facts
COVID-19 and Seasonal Flu Combination May Require Maternal-Fetal Specialist Care Click to Tweet
Burd’s team has developed several models of inflammation (maternal exposure to lipopolysaccharide and IL-1beta) and infection (Zika and cytomegalovirus, or CMV) to evaluate the impact of placental inflammation on fetal brain development and long-term sequelae. In murine models of intrauterine inflammation, the team established that inflammation, primarily through maternal IL-1beta signaling at the placenta, leads to fetal neurotoxicity and long-term adverse perinatal sequelae. Those studies[ii] show both genetic and pharmacologic blockade of IL-1beta signaling ameliorate perinatal brain injury.
Burd’s collaborative studies in Pune, India, formed the basis for another NICHD-funded grant to study placental determinants of aberrant immune system formation. “We found that HIV-exposed but noninfected children are more likely to die from other infectious causes than HIV in their early childhood years,” she says. “We are now pursuing similar studies in COVID-19-infected pregnant women, identifying the role of increased maternal IL-1beta in adverse long-term outcomes of exposed neonates.”
To refer a patient or discuss a case, call 410-502-3200.
Early Tragedy Guides Career
Twenty years ago, Irina Burd lost her first child in utero after contracting a parvovirus infection. This tragedy led her to pursue a career in maternal-fetal medicine.
“My baby girl developed hydrocephalus before the stillbirth,” she says. “I was in medical school at the time, and that brought out my love for high-risk obstetrics. For every bad thing that happens to you in life, there’s always a silver lining. You look back and the one-time tragedy becomes your lifetime work. I now have two sons and a beautiful family.”
Burd splits her work between research and clinical pursuits, and every fourth day she provides on-call maternal-fetal medicine coverage for Howard County General Hospital, a Johns Hopkins Medicine member hospital. “I get to work at the mothership in East Baltimore and at our community hospital; that’s the beauty of working at Johns Hopkins,” she says. “That plus the teaching, too.”
As director of the Integrated Research Center for Fetal Medicine, Burd brings together scientists and physician-scientists from across Johns Hopkins’ schools of public health, engineering and medicine to move maternal-fetal health toward personalized medicine.
“In maternal-fetal medicine, and in obstetrics overall, we really lack physician-scientists,” she says. “We are creating the infrastructure at Johns Hopkins for bringing the next generation of scientists and physician-scientists on board so we can move science forward. Educating the next generation of physicians and doing research in maternal and child health is the number one priority to me.”
- [i] Novak CM, Lee JY, Ozen M, Tsimis ME, Kucirka LM, McLane MW, Xie L, Kelleher M, Xie H, Jia B, Lei J, Burd I. Increased placental T cell trafficking results in adverse neurobehavioral outcomes in offspring exposed to sub-chronic maternal inflammation. JCI Insight. 2019 Feb 28;4(7):e122678. doi: 10.1172/jci.insight.122678. eCollection 2019 Apr 4.JCI Insight. 2019. PMID: 30944243
- [ii] Lei J, Vermillion MS, Jia B, Xie H, Xie L, McLane MW, Sheffield JS, Pekosz A, Brown A, Klein SL, Burd I.Lei J, et al. Among authors: Burd I. IL-1 receptor antagonist therapy mitigates placental dysfunction and perinatal injury following Zika virus infection. JCI Insight. 2019 Feb 28;4(7):e122678. doi: 10.1172/jci.insight.122678. eCollection 2019 Apr 4.JCI Insight. 2019. PMID: 30944243
- Leitner K, Al Shammary M, McLane M, Johnston MV, Elovitz MA, Burd I. Leitner K, et al. Among authors: Burd I. IL-1receptor blockade prevents fetal cortical brain injury but not preterm birth in a mouse model of inflammation-induced preterm birth and perinatal brain injury. Am J Reprod Immunol. 2014 May;71(5):418-26. doi: 10.1111/aji.12216. Epub 2014 Mar 5.Am J Reprod Immunol. 2014. PMID: 24592965
- Tsimis ME, Lei J, Rosenzweig JM, Arif H, Shabi Y, Alshehri W, Talbot CC, Baig-Ward KM, Segars J, Graham EM, Burd I. Tsimis ME, et al. Among authors: Burd I. P2X7 receptor blockade prevents preterm birth and perinatal brain injury in a mouse model of intrauterine inflammation. Biol Reprod. 2017 Aug 1;97(2):230-239. doi: 10.1093/biolre/iox081.Biol Reprod. 2017. PMID: 29044426