
NeuroLogic
November 18, 2013
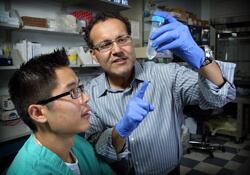
But a tissue type often considered a bodily pariah could hold the key to new and more effective glioblastoma treatments. In laboratory studies, Johns Hopkins researchers led by neurosurgeon Alfredo Quinones-Hinojosa have found that stem cells from a patient’s own fat may have the potential to deliver new treatments directly into the brain after the surgical removal of glioblastoma tumors.
The investigators say mesenchymal stem cells (MSCs)—multipotent stem cells that can be isolated from a variety of tissues, including bone marrow, muscle and adipose tissue—have an unexplained ability to seek out damaged cells, such as those involved in cancer. This quality may provide clinicians a new tool for accessing difficult-to-reach parts of the brain where cancer cells can hide and proliferate anew. Furthermore, harvesting MSCs from fat is less invasive and less expensive than getting them from other sources.
“The biggest challenge in brain cancer is the migration of cancer cells,” says Quinones-Hinojosa. “Even when we remove the tumor, some of the cells have already slipped away and are causing damage somewhere else. Building on our findings, we may be able to arm a patient’s own healthy cells with the treatment needed to chase down those cancer cells and destroy them.”
For their experiments, Quinones-Hinojosa and his colleagues bought human MSCs derived from both fat and bone marrow, and also isolated and grew their own stem cell lines from fat removed from two patients. Comparing the different cell lines, they discovered that all proliferated, migrated, stayed alive and kept their potential as stem cells equally well.
This was an important finding, Quinones-Hinojosa says, because it suggests that a patient’s own fat cells might work as well as any to create cancer-fighting cells. The MSCs, with their ability to home in on cancer cells, might be able to act as a delivery mechanism, bringing drugs, nanoparticles or some other treatment directly to the cells.
Ideally, he says, if MSCs work, a patient with a glioblastoma would have some adipose tissue removed from any number of locations in the body a short time before surgery. The MSCs in the fat would be drawn out and manipulated in the lab to carry drugs or other treatments. Then, after surgeons remove the brain tumor, they could deposit these treatment-armed cells into the brain in the hope that they would seek out and destroy the cancer cells.
“Essentially these MSCs are like a ‘smart’ device that can track cancer cells,” Quinones-Hinojosa says. “Eventually, we may be able to use this quality to turn what some people would rather do away with into a new way to attack this disease.”
Information: 410-550-3367

