
Cardiovascular Report
January 6, 2014
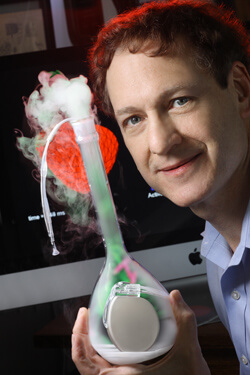
David Kass’ lab played a key role in developing CRT for use in patients in the late 1990s. Since then, Kass and colleagues have been running the discovery clock backwards to reveal how CRT strengthens heart muscle while making it beat in a coordinated fashion.
In a recent study described in the Journal of Clinical Investigation, the scientists showed that CRT changes heart cells so they can contract more forcefully. They also identified an enzyme that mimics the effect of CRT without use of the device.
“These discoveries potentially give us new pathways to benefit more heart failure patients—not only those whose hearts beat out of sync, but also those who do not qualify for CRT therapy,” says Kass.
The researchers used an animal model of heart failure with dyssynchrony and also examined the impact of CRT on the heart. By studying isolated muscle tissue and muscle cells, they examined the relationship between contraction and the calcium that triggers it. In dyssynchronous hearts, force from the muscle cells and the level of calcium needed to generate contractions were very much reduced. CRT improved contraction force more than calcium, which led to the discovery that CRT had increased the muscle’s sensitivity to calcium.
Calcium sensitivity is a property of the proteins that form the contracting “engine” of muscle, so the investigators next examined how these proteins had been biochemically altered by CRT. After ruling out all the known ways this might have occurred, they tested for changes in more than 150 proteins and discovered that CRT specifically modified 13 of them.
“Once we discovered which proteins were being altered, we identified an enzyme likely responsible for these changes,” says lead author Jonathan Kirk, a postdoctoral fellow. The enzyme, GSK-3 beta, converted the behavior of muscle cells beating out of sync to what looked like heart cells that had received CRT.
They also found that although GSK-3 beta was inactive in muscle from a failing and dyssynchronous heart, it was reactivated by CRT. When that happened, the enzyme altered the motor proteins so that they generated greater force using the same amount of calcium-based activation.
“It had never been shown before that GSK-3 beta could modify motor proteins in the heart to make them more sensitive to calcium. It is surprising that this same type of effect can be produced by CRT,” says Kass.
Kass and colleagues previously showed that CRT enables heart muscle to respond to hormones, such as adrenaline, to stimulate pumping ability.

