Though it’s well known by surgeons and others that robotic surgery offers benefits such as smaller incisions and reduced hospitalization time and postsurgical pain, clinicians learning to use surgical robots have a steep learning curve, says Gina Adrales, director of the Division of Minimally Invasive Surgery. She and her colleagues aim to improve this curve through innovative training techniques and a newly developed, wearable device.
— Gina Adrales
When a surgeon operates a machine that is away from the patient, “there’s no haptic feedback with the most widely used robotic platform,” Adrales explains. “Normally, when you do open surgery, you can feel how instruments interact with tissue. You get feedback through your hands and the instruments about how firm tissue is, or how much tension you are putting on something — such as a suture when you’re tying it.”
To compensate during robotic surgery, she says, surgeons need to develop what’s called haptic visual acuity — the ability to view the operating field on a screen and determine how much tension to exert and how to maneuver the robotic arms’ tools to achieve optimal results.
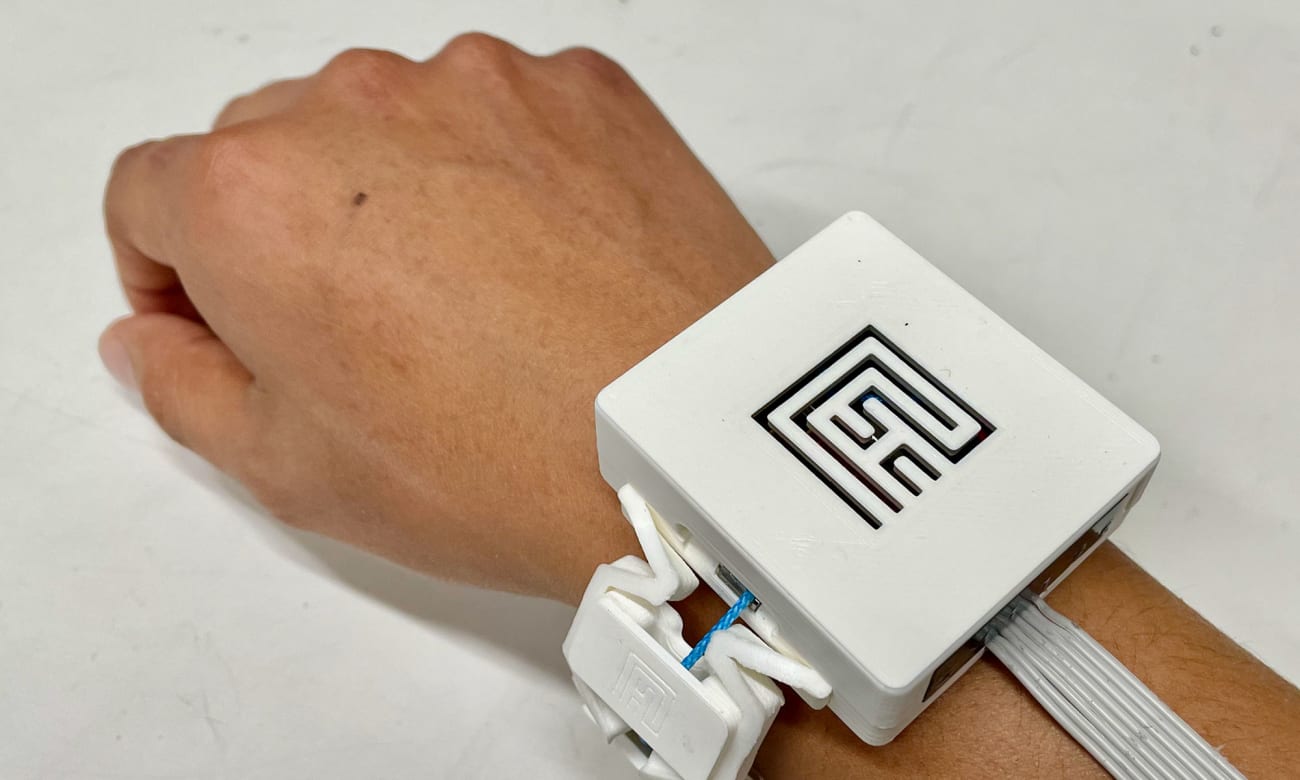
To augment that skill for surgical residents and other trainees, Adrales has been working with experts at the Johns Hopkins Malone Center for Engineering in Healthcare. She has partnered with Jeremy Brown, the John C. Malone assistant professor of mechanical engineering, who developed a sensor device, worn on the wrist, which vibrates in response to the amount of force applied on tissue during surgical training cases at the Minimally Invasive Surgical Training and Innovation Center (MISTIC). The greater the force applied, the stronger the vibration.
“We want to determine if use of this technology helps accelerate the learning process and allows surgeons to correlate the force applied with what they see visually while using the robot,” Adrales says. “Can we make the learning process a little more efficient so that people can ascend their learning curve a little faster through training and enhance the safety of patients in the operating room when they’re actually doing surgery?”
Initially, tools such as this can slow learning down as users learn to incorporate feedback, but “our premise is that we think it’s going to enhance the training process overall,” she says. The next phase of study will evaluate how well using the device can translate to better operative performance and patient safety.
And, because expert surgeons aren’t always available to proctor trainees practicing on models at MISTIC, another project, led by Swaroop Vedula, a doctor with surgical training and an assistant research professor, is working to incorporate an automated coaching feature that would provide expert feedback through text on the screen, so novice surgeons can learn in an environment that is more similar to an operating room. Training programs as they are now might tell users that they’re on or off the mark when inserting a needle, for example, but not specify the way they are making errors, Adrales says.