
HeadLines
June 13, 2017
In January 2016, a routine physical revealed a swollen lymph node on the left side of Matt Harcourt’s neck. Although the 46-year-old father of three had no symptoms, a biopsy by a local ear, nose and throat specialist near his home in Bethesda led to a diagnosis of squamous cell carcinoma of the oropharynx, or head and neck cancer. When he reached out to his friends for advice, they suggested seeing someone affiliated with Johns Hopkins Medicine.
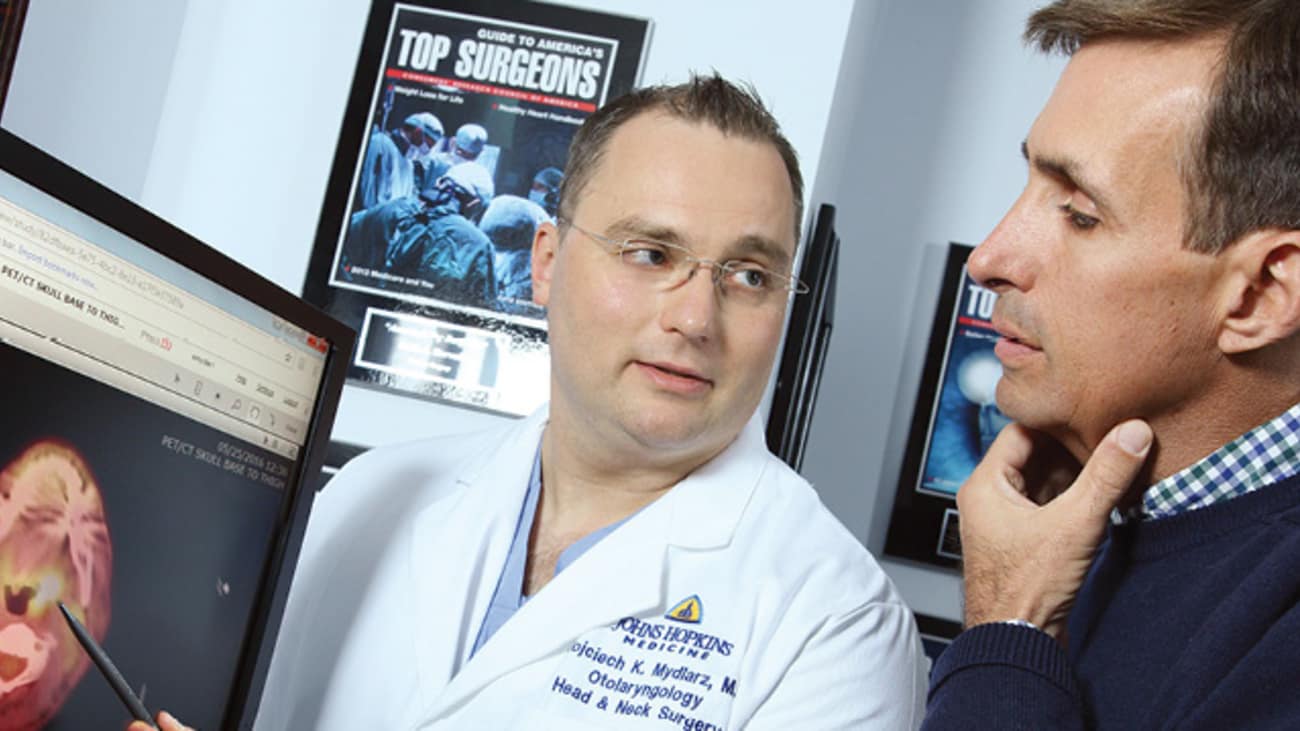
His first appointment was with Wojtek Mydlarz, a Johns Hopkins head and neck surgeon who practices at Suburban Hospital in Bethesda. On the same day, Harcourt also saw Brandi Page, a radiation oncologist who specializes in head and neck cancer at the Johns Hopkins Kimmel Cancer Center radiation oncology practice in Bethesda. Nicholas Farrell, a medical oncologist in private practice in Bethesda, was also on the treatment team.
Mydlarz suspected that Harcourt’s cancer originated in his left tonsil, a hypothesis confirmed by a physical exam and biopsy. A PET scan revealed that the cancer had spread to some of the lymph nodes in Harcourt’s neck, making it less likely that surgical treatment would be curative without the addition of radiation and chemotherapy.
Mydlarz shared the case at head and neck tumor board conferences at Suburban Hospital and The Johns Hopkins Hospital, where team members discuss complicated cases. “Every head and neck cancer patient benefits from the expertise of all the Johns Hopkins specialists, whether they receive treatment locally or in Baltimore,” Mydlarz explains.
In early June, Harcourt began a seven-week course of daily radiation and weekly chemotherapy. Page used cutting-edge radiation technology to ensure his treatments were delivered with pinpoint accuracy. “Our goal is to avoid as many side effects of treatment as possible,” she says. “Our specialized radiotherapy staff, which includes a speech and swallow therapist as well as a clinical social worker and dietitian, works hard to ensure the best short- and long-term outcomes. It’s so important to have all of these care components available in one place close to home.”
For Harcourt and all of Suburban’s cancer patients, another benefit of staying close to home is the support of oncology nurse navigator Barbara Doherty. “On day one, Barbara introduced herself as ‘the person to go to when you don’t know where to go’ and that she is,” Harcourt says. “There wasn’t a question she couldn’t answer on the spot. Her expertise was invaluable.”
Today, all indications are that Harcourt’s treatment was successful, although he is still adjusting to the effects of the radiation on his voice, salivary glands and sense of taste. He is hopeful these side effects will improve in time and that he will soon be declared “cancer free.”
“While having cancer is a terrible experience, I can’t say enough great things about everyone involved in my care,” says Harcourt. “The physicians, nurses, and radiation and oncology technicians made the whole thing more bearable because of their knowledge and professionalism. They all chose this profession because they care about people and it shows.”

