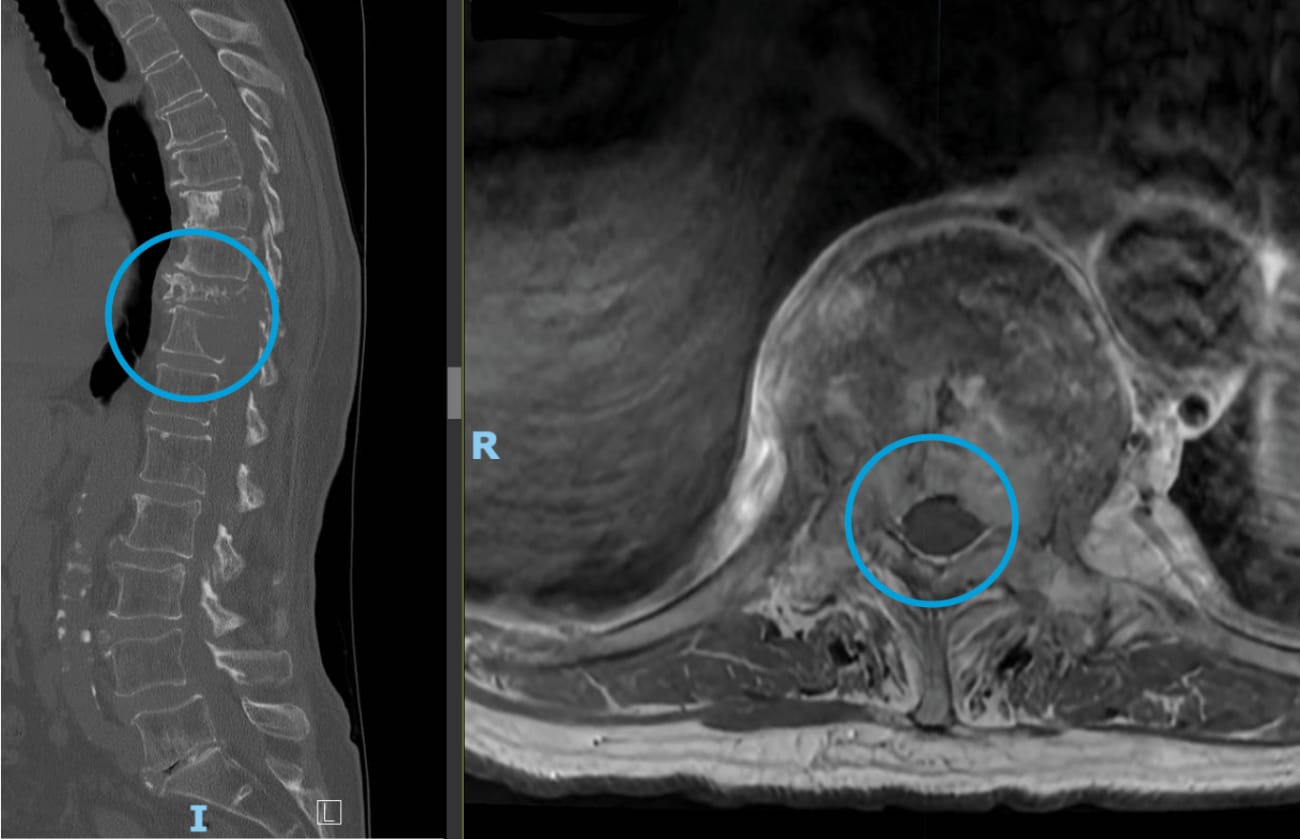
The patient, an active 80-year-old, had felt healthy for a dozen years after she had declined further treatment for breast cancer. But in late 2022, after undergoing hip replacement surgery, she developed back pain that became progressively worse. Initially suspecting complications from her recent operation, she tried to relieve the pain with exercise and stretching. But imaging showed something far more sinister: The breast cancer had metastasized to her thoracic spine, fracturing her T10 and T11 vertebrae, and invading her spinal canal.
A spine surgeon she initially met for a consult told her that open surgery to stabilize her spine and decompress her spinal cord would be the best option. But, the patient had an active life, and was the primary caregiver for a family member with a disability — being able to return to her regular lifestyle as quickly as possible was an important goal.
To see if that aim was within reach, she arranged for a second opinion with Daniel Lubelski, director of spine tumor surgery at Johns Hopkins, who offered that a minimally invasive surgical approach might be possible.
Avoiding open surgery could significantly reduce several of the risks associated with it, says Lubelski, such as excessive blood loss, infections and a long recovery time. The patient’s radiation oncologist, Kristin Redmond, and medical oncologist, Danijela Jelovac, supported this idea — but only if Lubelski was able to successfully remove the tumor to create at least several millimeters of margin between the spinal cord and vertebra, a requirement for the stereotactic body radiation therapy this patient would need afterward to treat her cancer.
In May 2023, Lubelski and his colleagues performed the surgery, assisted by a robotic navigation system. Utilizing the intraoperative navigation system, the surgeons placed the robot-guided screws to stabilize the patient’s spine, using carbon fiber screws instead of the usual titanium to minimize scatter and artifact on follow-up imaging studies. Then, Lubelski inserted a tubular dilator to carefully push muscle away from the affected area of the spinal column. To minimize damage to surrounding structures, he used an ultrasonic drill to cut away the tumor and decompress the spinal cord, rather than a traditional drill.
After three weeks, the patient began radiation therapy and systemic medical therapy for her cancer, taking both an estrogen modulator and a kinase inhibitor. Within months, she was walking unassisted and reported significant improvement in her mobility, pain and function. She had resumed her active lifestyle, and was able to care for her family member again — an outcome that likely occurred sooner due to the choice to take a minimally invasive approach rather than traditional open surgery, says Lubelski.
To refer a patient, please call 410-955-4424.