
Winter 2017
Fine-tuning Therapy for Multiple Sclerosis, Why Cystic Fibrosis Requires a Full-court Press, a Genetically Unique CF Patient, Tracking Moods Via Texts and More.
Fine-Tuning Therapy for Multiple Sclerosis
The complex autoimmune disease requires a full-court press.
Decades ago, there wasn’t much that physicians could do for people suffering from multiple sclerosis—except diagnose the illness and wish them luck. Now, there are 14 FDA-approved drugs and the promise of new therapies on the horizon.
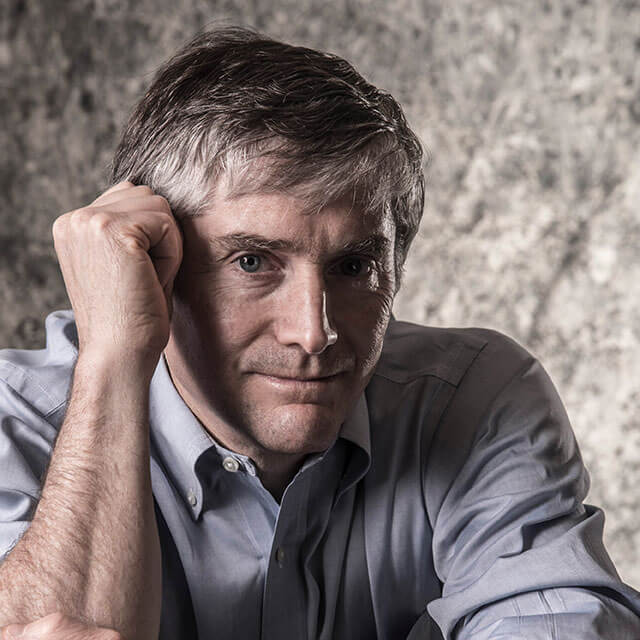
But Peter Calabresi, director of the Precision Medicine Center of Excellence (PMCOE) for Multiple Sclerosis, part of the Johns Hopkins inHealth initiative, notes that the often-degenerative illness, which causes lesions in the brain and disrupts the flow of information in the central nervous system, continues to take a terrible toll.
“We have drugs that put people with relapsing-remitting MS into long-term remission, but about half of the cases become progressive, and people end up in wheelchairs,” Calabresi says. Many lose their jobs or see their marriages unravel. “They don’t necessarily die directly of MS, but their lives may be devastated by it.”
Calabresi is working to change that by using advanced imaging and biomedical and statistical tools to better tailor treatments for MS patients. “The more layers of complexity you understand,” he says, “the more you can fine-tune the therapy.”
He has pioneered the use of optical coherence tomography (OCT), an imaging method widely used by ophthalmologists for eye exams, as a tool for monitoring MS.
Over the past decade, he and his colleagues have built a database of OCT retinal scans of more than 3,000 MS patients.
Tracking the progress of MS in the brain is difficult using established imaging techniques. But by using OCT, Calabresi and his team have been able to show that retinal degeneration is directly related to atrophy in the gray matter of the brain.

Thus, retinal scans—which are relatively fast, easy and inexpensive—can be used as stand-alone surrogates for brain damage in MS, providing important clues as to how quickly a patient’s disease is progressing.
Today, at the Johns Hopkins Multiple Sclerosis Center, which Calabresi directs, his patients are routinely given annual OCT and MRI scans. He’s now trying to improve the scans to the point where he can use the database to generate predictions of a patient’s condition five or 10 years out.
His clinic is also conducting genetic and metabolic research, which he hopes will bring each patient’s illness into sharper focus, allowing even more precise treatment. “That’s where I see us going, is just drilling down,” he says. “You don’t just have MS, you have a variant at a particular stage, and that means you’re likely to respond to a specific drug.”
Overall, by marshaling all the resources of the new PMCOE for Multiple Sclerosis, Calabresi aims to continually adjust treatment for his patients as their illness progresses, prescribing drugs and therapies with fewer side effects for patients likely to do well and stronger treatments for those at risk, all in an effort to maximize quality of life. “We’re not waiting five years to find out you’re in a wheelchair,” he says.
A Benefit from Vitamin D?
Multiple sclerosis is relatively common in the temperate climates of northern Europe and the Southern Hemisphere, and rare close to the equator. Neurologist Peter Calabresi says studies have found a strong correlation between the lack of sunlight exposure before puberty and the risk of developing MS.
Low levels of vitamin D, which is activated by exposure to sunlight, may be one factor in the illness. Studies have shown that people who have MS and low levels of vitamin D are more likely to have clinical or MRI disease activity.
Currently, patients with MS at Johns Hopkins are routinely tested for vitamin D levels, and there are ongoing studies by neurologist Ellen Mowry that are examining the use of vitamin supplements to treat MS.
“We’ve worked on vitamin D because it’s very appealing from a safety standpoint,” Calabresi says. So far, the research suggests that supplementing vitamin D may have benefits in regulating the immune response in MS, but that there may be a genetic link between MS and chronic low vitamin D levels that requires further investigation.
No ‘Simple’ Genetic Disease
Targeted therapies for CF involve genetic sleuthing—and more.
When cystic fibrosis was first identified in the 1930s, researchers reported that it followed the simple Mendelian rule for recessive traits: People who inherit a mutated copy of the gene for CF from one parent didn’t get the disease, but those who inherit copies from both parents did.
As it turns out, there was nothing simple about cystic fibrosis. Since the CFTR gene for the disorder was first discovered in 1989, researchers have found nearly 2,000 mutations, hundreds of which can cause illness. Since each gene can carry multiple mutations, there are millions of potential combinations of these gene variants. Add the effects of modifier genes, and environmental and behavioral factors to the mix, and a map of this “simple” genetic disease becomes a labyrinth.
Some patients with CF die in elementary school. “Other people are diagnosed with exactly the same genetic defect, and they live a fairly well-managed life into their 50s and 60s, have children. And it’s the same gene that’s been affected,” says Patrick Sosnay, assistant professor of medicine.
The disorder restricts the transport of chloride through ion channels at the surface of cells, affecting the pancreas, gut and sweat glands. But its effects can be most devastating in the lungs, where it causes a buildup of thick, sticky mucus that clogs the airways and serves as a nursery for bacteria and viruses.
To target CF in all its guises, Sosnay and Garry Cutting, the Aetna U.S. Healthcare Professor of Medical Genetics, have spent nearly a decade working on Johns Hopkins’ CFTR2 Project—a database of 88,000 CF patients from the U.S. and around the world.
Currently, there are about 320 adults and 250 children being treated for CF at Johns Hopkins, says Noah Lechtzin, director of Johns Hopkins’ adult CF program. Each is screened for mutations in their CF genes to predict the likely course of the disease and to flag those patients who are candidates for drug trials. A patient’s DNA may also be tested, using epithelial cells grown in the lab, to determine if he or she can benefit from either of the two currently available drug therapies.
Given how dramatically CF can vary and how expensive the drugs are, traditional large-scale human testing of new CF drugs may not be possible, so Sosnay says he hopes the Food and Drug Administration will adapt its approval process to reflect this. “We really want a way to use lab-based evidence that says, ‘Hey, this drug is going to work, and it’s promising enough that you should license it,’” he says.
As advances in genetics, data analysis and biomedicine produce more detailed pictures of disease, Sosnay says, patients will increasingly be sorted by the type of treatment they respond to—their “theratype,” or therapeutic type—rather than by broad disease categories.
In some cases, genes will mainly determine the theratype. But in others, the symptoms of an illness can be carefully and continually monitored to decide the best course of treatment. For example, people with cystic fibrosis have abnormally high chloride levels in their perspiration. Traditionally, they have come into the clinic for regular “sweat tests”—a procedure originally developed at Johns Hopkins—which are helpful for charting the course of their illness.
Through a Johns Hopkins inHealth initiative, Cutting is currently working with a team of Johns Hopkins engineering students and faculty members to develop a wearable monitor for continuously measuring skin salt levels. These devices are designed to provide a picture of how these salt levels vary over time and tell how patients are faring between sweat tests. Currently, says Cutting, “We don’t know how patients respond to a drug dose. All kinds of things remain unanswered because we don’t have a way to continually measure and get numbers.” The wearable sweat sensor aims to make it easier for physicians to provide personalized treatment programs—and identify which patients might most benefit from expensive and potentially hazardous treatment.
“We have these novel CF treatments that are risky,” explains biostatistician Scott Zeger, a co-director of Johns Hopkins inHealth. “So if you know a person is going to be one of those with a more normal life, maybe it’s good to do watchful waiting and active surveillance, versus an immediate intervention.”
Apps: Better Health Made Easy
Accessible from smartphones, watches and tablets, apps are a boon to precision medicine. Among the many apps developed at Johns Hopkins, here are three that promise to be real game changers.
Helping with Heart Attack Recovery
Nationwide, one in five cardiac patients is readmitted to the hospital within 30 days. “They leave without the guidance, information and skill-building they need to get a healthy start,” says Francoise Marvel, a third-year internal medical resident and soon-to-be chief resident.
Marvel is leading a team of Johns Hopkins physicians, nurses, designers and engineers who are collaborating with Apple on an app designed to empower heart attack patients in their recovery. The app, called Corrie (“cor” is Latin for heart), works with Apple Watch and would be the first cardiology app in CareKit, Apple’s new framework for medical applications.
Corrie monitors a patient’s heartbeat, blood pressure and exercise, creating a record for patients and their doctors. It also alerts users when it’s time to take medications, and it pings if they have been sitting a long time and would benefit from a walk. Through Corrie, users can also schedule follow-up appointments and learn about heart health through animated videos.
“It’s like a digital health buddy to keep patients on track,” says Marvel.
She began developing the app in 2014 with support from Johns Hopkins Technology Ventures and grants. The project gained momentum in 2016, when Marvel teamed with preventive cardiologist and mobile health expert Seth Martin, and with Whiting School of Engineering students Matthias Lee and Gavi Rawson.
For a pilot study, Apple donated 200 Corrie-equipped smartwatches to The Johns Hopkins Hospital and Johns Hopkins Bayview Medical Center. Cardiac patients at those hospitals now receive the watches the day after they are admitted and keep them for 30 days after discharge. If the pilot shows Corrie can help those patients improve their health and prevent readmissions, the app could be available to cardiac patients at other hospitals within the next year.
Improving Physician-Patient Communication
If you’re a patient who will be undergoing a procedure, you’ve likely experienced it: sitting across from your doctor, unsure if you’ve forgotten to ask something crucial. If you’re a doctor, you know the other side of this equation: trying to help patients who are confused about a procedure and eager for more information.
Enter Doctella, an app to improve communication between doctors and their patients. Based on Johns Hopkins’ pioneering use of safety checklists, the app provides patients with checklists of questions to ask before, during and after a medical procedure.
Doctella is free for patients and many doctors encourage their patients to use it.
When patients create a profile, they can then personalize the checklists with their notes and answers. Physicians can create a personalized Doctella page with customized answers and videos on subjects such as how to change a dressing. They can also set Doctella to send patients reminders about taking their medications.
The app was created by Peter Pronovost, director of the Armstrong Institute for Patient Safety and Quality; anesthesiologist Asad Latif; and former Johns Hopkins surgeon Adil Haider.
Tracking Moods via Texts

For psychiatrist Adam Kaplin, staying on top of his patients’ moods is important. But asking them to recall their moods just wasn’t working.
“I can’t remember what I had for dinner three days ago,” says Kaplin. “How can they remember what their mood was like a week ago? Even when it’s complete, the traditional chart often delivers bad data.”
In 2010, Kaplin met with Remedy Health Media, a health information technology company, and shared his idea for a better system: one that would text patients to ask them to rate their mood each day. People would text a response using a scale from one to 10, and the information would be stored on a HIPAA-secure website.
The company loved his idea. It soon licensed the technology from Johns Hopkins Medicine and built the system. Today, there are more than 15,000 registered users of mood247.com, including patients, doctors and family members.
Kaplin has found that patient participation in mood charting—rating and recording how they feel each day—skyrocketed from 10 to 90 percent. The traditional paper charts used for mood monitoring are often backfilled while patients sit in the waiting room before their appointment.
He believes the success of mood247.com stems from the fact that it’s based on something people already use—text messages.

A Genetically Unique CF Patient
Off-the-rack medicine for cystic fibrosis would never have suited Juliet Page.
When Page was a girl growing up on Long Island, New York, in the 1960s and 1970s, she struggled with recurring bouts of bronchitis, pneumonia and other lung infections. “I could never catch a cold and then be over it in two or three days like a normal person,” she says.
Through marriage, graduate school and her career as an aerospace engineer, Page’s condition remained a mystery. Recurring, persistent lung ailments are a classic sign of cystic fibrosis, but her symptoms did not tick all the boxes for the disease.
Finally, in her 40s, she developed a tenacious bacterial lung infection. She came to Johns Hopkins, where a team is seeking to identify every one of the thousands of cystic fibrosis mutations that exist and to develop methods for treating those mutations. Page’s testing in 2008 showed that she was a genetically unique CF patient. It found that she carries three CF genes—one copy of F508del, the mutation carried by 70 percent of cystic fibrosis patients; another called G178E, which is so rare it hasn’t been studied; and a third that has only been found in her and one other person.
Page’s illness finally had a label, cystic fibrosis—but the first effective treatment didn’t come until 2012.
That’s when the FDA approved the drug ivacaftor for 2 to 4 percent of patients with a rare mutation—but not any of those she carried. Her Johns Hopkins physician, Patrick Sosnay, a member of the Johns Hopkins Cystic Fibrosis Center, thought she might benefit from the drug anyway. The CF team set up a one-month trial of the drug, which can cost $300,000 a year, monitoring chloride levels on her skin. (CF patients have two to five times the normal level of chloride in their sweat.)
When the tests showed striking reduction in sweat chloride, Page’s insurance company agreed to pay for her treatment.
“It’s been life-changing for me,” says the engineer, who lives with her husband and daughter in Annapolis. “I have only caught a couple of colds a year, and I’m over them in three or four days like a normal person. This is amazing.”

